 What is quality? Is it service? Is it amenities? Is it results? In previous issues of CAPsules, we have looked at Improvement Activities (IA) and Advancing Care Information (ACI). We have reflected that, while we have always managed to metrics, the continuing evolution of payment reform as evidenced by the Quality Payment Program (QPP) has at times felt like a rockslide bearing down on us. But amid our eye rolling, hand wringing, and deploying of expletives, we come to see that underlying improvement activities, advancing care information, and quality are our old friends communication and documentation in the many forms they take.
What is quality? Is it service? Is it amenities? Is it results? In previous issues of CAPsules, we have looked at Improvement Activities (IA) and Advancing Care Information (ACI). We have reflected that, while we have always managed to metrics, the continuing evolution of payment reform as evidenced by the Quality Payment Program (QPP) has at times felt like a rockslide bearing down on us. But amid our eye rolling, hand wringing, and deploying of expletives, we come to see that underlying improvement activities, advancing care information, and quality are our old friends communication and documentation in the many forms they take.
In May, we looked at three high-weighted activities that could contribute the most to your IA score: population management through personalized, periodically reviewed care plans; collection and followup on patient experience and satisfaction data with a plan of improvement where indicated; and patient safety and practice assessment, especially with regard to prescribing practices.
In June, we looked at the required measures in ACI: monitoring the safety and security of the electronic health record system; using electronic communications with patients with appropriate safeguards and informed consent; having and using a process for follow-up and follow through to improve patient understanding of their plan of care, improve adherence to the plan, and achieve the desired outcome; and e-prescribing.
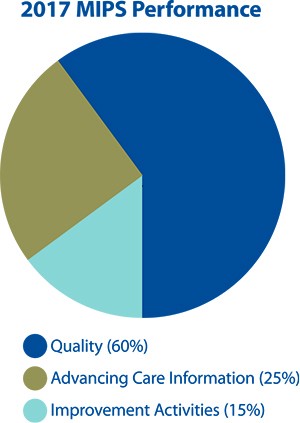
This month, we consider quality and the measures that will contribute to that important 60 percent of the MIPS 2017 performance score.
If we persist in our approach of taking credit for what we do best, based on years of practice and thousands of patient/family interactions, we can look at the list of measures and select measures that best fit the practice: six measures, including one outcome measure and one high-priority measure. There are 300 to choose from. We can refine our search by specialty. There are 30 specialty measure sets. Or by high priority or by data submission method.
What follows is a sample list of measures that might reflect activities in a general medical practice. As you read through them, notice how they link up with Improvement Activities and Advancing Care Information. A striking feature of the Quality Payment Program is its acknowledgement of the dynamic relationship among all the components of the comprehensive patient-centered care CAP member physicians and practitioners provide.
Biopsy follow-up: Percentage of new patients whose biopsy results have been reviewed and communicated to the primary care/referring physician and patient by the performing physician.
Breast cancer screening: Percentage of women 50 to 74 years of age who had a mammogram to screen for breast cancer.
Care plan: Percentage of patients age 65 years and older who have an advance care plan or a surrogate decision maker documented in the medical record or documentation in the medical record that an advance care plan was discussed but the patient did not wish or was not able to name a surrogate decision-maker or provide an advance care plan.
Closing the referral loop: Percentage of patients with referrals, regardless of age, for which the referring provider receives a report from the provider to whom the patient was referred.
Hypertension-improvement in blood pressure: Percentage of patients age 18 to 85 years with a diagnosis of hypertension whose blood pressure improved during the measurement period.
Controlling high-blood pressure: Percentage of patients 18 to 85 years of age who had a diagnosis of hypertension and whose blood pressure was adequately controlled (<140/90mmHg) during the measurement period.
We were recently asked what can providers who are not participating – or are not fully participating in 2017 – do to ensure that they are prepared for 2018?
Our answer: Practitioners should consult with colleagues and take advantage of the free support services available to understand where their practices stand in relation to the reporting structure, measures, and requirements. We are convinced that the gifted and dedicated practitioners in CAP will get organized to demonstrate to themselves, to CMS, and to the wider community just how good they are – and get paid as well!
Watch for updates from CAP as the Quality Payment Program evolves and new information and resources become available.
Carole Lambert is Vice President, Practice Optimization for CAP. Questions or comments related to this article may be sent to clambert@CAPphysicians.com.
SOURCES
CMS Proposes Quality Payment Program Updates to Increase Flexibility. Health Services Advisory Group, accessed June 21, 2017.
Preparing for MIPS in the Small Group Practice. Impaq International webinar, June 8, 2017.
qpp.cmc.gov/measures, accessed June 5, 2017.
Weber, S. 11 Ways Small Practices Can Comply with MACRA. Physician Practice, UBM Medica Network, accessed April 14, 2017.