When asked, “What keeps a hospitalist up at night?” Jeff Shapiro, MD, hospitalist at Citrus Valley Health Partners-Foothill Presbyterian Hospital answered, “Well, I can tell you it used to be medication reconciliation” (med rec).
“Before re-engineering our process, we had concerns about the quality and accuracy of the original medication list,” Dr. Shapiro says. “That list is the basis of safe prescribing. If a patient is admitted and needs to continue on anticoagulants or is taking something that might interact with what I plan to prescribe, I need to know about it! In the past, we did our best with our time and resources, but now we have dedicated pharmacy technicians performing medication reconciliation—a clear process with clear ownership and accountability—as well as outcome data to support that the list is complete and accurate. I’m definitely sleeping better!”
Dr. Shapiro’s concerns are supported by an abundance of data concerning medication risks. As the mainstay therapy of modern medicine, medication errors represent the most common type of patient safety error: the average hospitalized patient is subject to at least one medication error per day,(1) about 20 percent of which will result in harm.(2)
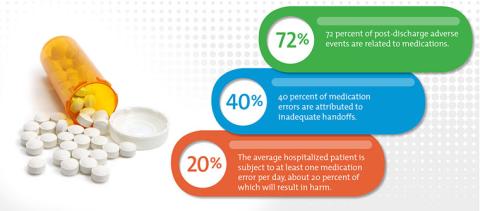
The risk is augmented during care transitions – 40 percent of medications errors are attributed to inadequate reconciliation during handoffs at admission, transfer, and patient discharge; and 72 percent of post-discharge adverse events are related to medications.(3) Although conservative prescribing, improved patient education, and technological advances such as barcoding and CPOE are certain to improve medication safety, a reconciled medication list is considered the cornerstone of prevention. Capturing an accurate and complete medication list, reviewing it, and ensuring its accuracy and appropriateness at every single transition point, is essential to patient safety.
The Joint Commission defines medication reconciliation as a five-step process:
1) develop a list of current medications;
2) develop a list of medications to be prescribed;
3) compare the medications on the two lists;
4) make clinical decisions based on the comparison; and
5) communicate the new list to appropriate caregivers and to the patient.
Seems straightforward, right?
But medication reconciliation has never been simple and remains one of the single greatest process improvement challenges in health care — from the archeological feat of piecing together an accurate patient medications list from multiple, incomplete sources, to defining and enforcing the respective roles of doctors, nurses, and pharmacists across a myriad transition points and clinical settings. Historically, med rec has always seemed, well, a bit of a wreck. Even the Joint Commission, who named medication reconciliation as a National Patient Safety Goal for hospital accreditation in 2006, mercifully simplified its original 17-element goal to five elements of performance—acknowledging the “good faith efforts” of professionals involved in capturing an accurate and complete medication list.
One Hospital’s Improvement Story
“Obtaining an accurate medications list when the patient first presents is the foundation of all safe prescribing that follows. But obtaining that original list is painstaking work,” says Dr. Ed Jai, PharmD and Corporate Director of Pharmacy for Citrus Valley Health Partners. “You’re relying on the patient’s memory—and that’s often the memory of someone who may have cognitive deficits, low health literacy, or even someone who isn’t feeling well enough to clearly recall their medications,” he explains. “Or, you’re relying on a previous medications list that may or may not be current and accurate. Relying on any one source may only tell part of the story. Doing it well means approaching med rec like an investigation and drawing on a number of sources — interviewing the patient and family, contacting the patient’s local pharmacy or his or her primary care provider, searching pharmacy databases, or relying on family to bring in the patient’s medications. The obvious issue here is that nurses and physicians are far too busy with procedures and patient care to do all of this extra work.”
“We knew we needed to improve, but our first goal was to really understand where we stood and to capture accurate baseline data for our pre-implementation process,” says Dr. Jai. “This is a very labor intensive process.”
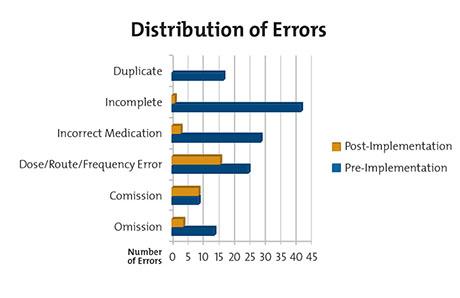
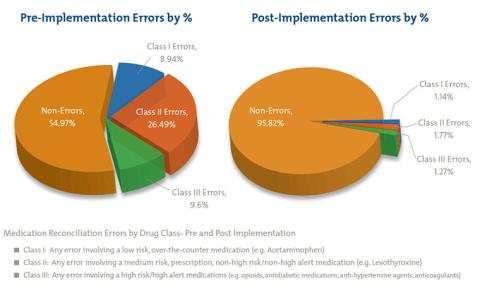
To establish baseline data, 30 patient profiles with prior-to-admission medications were subjected to expert review by pharmacists whose job it was to ascertain the accuracy of the lists and to identify any unintended discrepancies between what was documented and what should have been documented. These “unintentional discrepancies” include such errors as: medication omissions, or omitting a medication that the patient takes; commissions, or adding a medication the patient does not take; dose, route and frequency errors; and incorrect and incomplete medications. Pre-implementation, the reconciliation accuracy rate was about 55 percent, compared to an astonishing 96 percent, post-intervention.
The Path to Improvement
Under Dr. Jai’s direction and the expertise of a multi-disciplinary team, Citrus Valley embarked on a year-long quality improvement project to improve accuracy and reduce the error rate in their medication reconciliation process. Using “best-practice” research and Lean Six Sigma principles, the team trained and deployed pharmacy techs to perform medication reconciliation in two of their hospital emergency departments. Their results were truly impressive: They reduced their overall error rate by nearly 40 percent and increased their accuracy rate for all medications to almost 96 percent. The greatest gains were in reducing the percentage of errors associated with “class III” high-risk medications like narcotics, antibiotics, and anticoagulants, where unintended discrepancies are associated with increased likelihood of patient morbidity and mortality. Errors for this class of medications were reduced from 9.60 percent to 1.27 percent. In addition, the human resource savings was substantial (and greatly appreciated) by physicians and nurses who were spared countless hours of additional work and given more time for direct-patient care.
Expanding the Role of the Pharmacy Technician
“Some of the literature showed very promising results using pharmacy techs to conduct the initial medications reconciliation interview,” says Dr. Jai. The improvement team identified pharmacy techs with an interest in direct patient interaction and provided intensive training to prepare them for their new role. He adds, “There’s a definite strategy to interviewing patients. You want to ask questions in a way that triggers memory.
It’s important to use both open-ended and closed-ended questions, and to pick up on clues in the record. For example, if there’s a prescription for glucose test strips, the next question would be to ask if the patient is taking insulin.” To help technicians perfect their interviewing and investigation skills, the team provided formal training, including simulation exercises and feedback and coaching from direct observation. Additionally, technicians are provided support materials, to guide them when evaluating information from different sources.
It’s All About the Process: Ongoing Measuring and Monitoring
“To ensure that our process continues to yield the best outcomes, we continue to analyze several process measures including tracking start to complete time, recording allergies, classifying medications, and tracking whether the technician inquired about OTCs and supplements, the completeness of the order, as well as the number of medication sources used by the technician,” says Dr. Jai. “Most importantly, the technician must carefully document any noted discrepancies among sources. For example, the patient’s medication bottle may state he is taking 5 mg of an antidiabetic agent, when the patient actually takes 2.5 mg due to a previous hypoglycemic event.” These discrepancies are then reviewed and resolved by the pharmacist. The end result is a list the prescribing physician can rely on with a high degree of confidence.
In addition to fantastic outcome measures, Jai commented that pharmacy technicians have experienced a very satisfying expansion in their roles. “I think the technicians understand that their work is integral to the success of the team in safely treating the patient,” he notes. “Physicians and nurses are thrilled to have the extra support and an accurate and complete medications list. Everyone wins – especially the patient!”
Ed Jai, PharmD, would like to acknoweledge, Paul Morris, PharmD, Clinical Coordinator, for leading the Medication Reconciliation initiative at Citrus Valley Medical Center-Queen of the Valley, and for providing the data analysis.
If you have questions about this article, please contact us. This information should not be considered legal advice applicable to a specific situation. Legal guidance for individual matters should be obtained from a retained attorney.
1. Institute of Medicine. Preventing medication errors. Washington, DC: National Academies Press; 2006.
2. Rozick JD, Howard RJ, Justeson JM, et al. Patient Safety standardization as a mechanism to improve safety in health care. JT Comm J Qual Saf. 2004; 30(1):5-14.
3. Forster AJ, Clark HD, Menard A, Dupuis N, Chernish R, Chandok N, et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004; 170(3):345–349.