Diagnostic delays can be costly and harmful to patients. Although delayed diagnosis can occur in any medical specialty, primary care is at a significant risk for delayed diagnosis because it is where many initial and ongoing patient-doctor encounters occur.¹ One example of delayed diagnosis in the primary care setting was seen in a recent Pennsylvania case.
In 2012, a patient presented to her primary care physician (PCP) with complaints of mid-back pain and tingling in her ribcage that lasted six days.2,3,4 The PCP informed the patient to monitor her back symptoms and to notify him if her symptoms worsened or failed to improve.2,3,4 In March 2014, the patient saw her PCP with complaints of fatigue and back pain that occasionally woke her up.2,3,4 At the beginning of 2016, the patient reported tingling and sensory changes in her right foot and the PCP referred the patient to a podiatrist.2,3,4 However, despite the referral, the patient did not see the podiatrist until seven months later. The podiatrist conducted an evaluation and noted the patient had reported numbness radiating down her leg.2,3,4 As a result of the numbness, the patient was referred to neurology, but did not follow up with the neurologist.2,3,4 In October 2016, the patient saw her PCP for bilateral knee pain with swelling in the back of the left leg and more pronounced tingling sensation in her feet.2,3,4 Again, the patient delayed in following up with the neurologist and did not schedule an appointment until a month later.2,3,4
In January 2017, the patient was finally seen by a neurologist, who discovered the patient had an evolving spinal cord lesion.2,3,4 The patient filed a suit against her PCP and multiple healthcare entities.2,3,4 Subsequently, the jury awarded the patient one of the largest Pennsylvania medical malpractice verdicts at $19.7 million.2,3,4 This verdict was rendered because of the delayed diagnosis that resulted in the patient having incontinence, pain, and a partial loss of mobility.2,3,4
Further, despite the jury finding the patient 6% negligent, the physician was still found liable because of the failure to order radiological testing sooner and for not referring the patient to a neurologist when the patient first reported her symptoms.2,3,4 On the surface, the contributing factors to the patient’s outcome may appear to be the nexus of both the patient’s and physician’s actions. However, diagnostic delays are generally connected to multiple causal factors and not just individual factors. These factors include system factors and implicit bias.5
System Factors
Healthcare is a system that is highly dependent on humans and therefore requires comprehension of human performance within the system. The Sharp End Model depicts how systems can contribute to faulty diagnosis and overall performance outcomes.6
Figure 1: The Sharp End Model
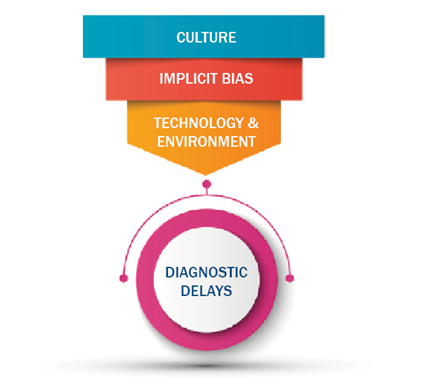
The funnel represents the clinical decision-making system, and the end point of the funnel is reflective of the intricate workings of these factors that contribute to diagnostic delays.6 Clinical decision making is a complex process. It involves a system of people, technology, and equipment that facilitates decision making. The awareness of such factors can help with recognizing that diagnostic delays are rarely ever caused by a singular factor. Therefore, mitigating the risk of diagnostic delays requires an understanding of a factor that is often overlooked, which is implicit bias.
Implicit Bias
Although not specifically stated in this case, could the fact that the patient was a middle-aged Hispanic female have unconsciously influenced the provider’s management of this case? The patient alleged that the physician failed to take her symptoms seriously and therefore failed to respond adequately to her complaints. Implicit bias refers to the attitudes and beliefs about race, ethnicity, age, ability, gender, or other characteristics that operate outside our conscious awareness and affect our actions and decisions.7 Implicit bias is hidden and is often activated involuntarily without awareness.8 Implicit bias can lead to diagnostic delays because it can cause a provider to not objectively appreciate a patient’s symptoms. Implicit bias can also impact communication and the type of tests or referrals ordered.8
Figure 2: Strategies to Address Implicit Bias9
|
Strategy |
Impact |
|
Implement processes that limit clinicians from cognitive overload caused by time pressures, inadequate staffing, and overcrowding |
Lowers cognitive stress and helps prevent the trigger of bias |
|
Provide implicit bias training |
Increases awareness of own biases and how |
|
Promote racial diversity throughout your organization |
Supports a culturally rich and diverse organization that can help with recognizing and eliminating bias |
Strategies to combat implicit bias include limiting cognitive overload, education, and promoting diversity within your organization. Through such actions, you can help prevent biased thinking.
Key Takeaways
The Pennsylvania verdict shows that despite patients’ lack of follow through, physicians can still be held accountable for diagnostic delays. Therefore, it is important to appreciate that diagnostic delays are not linked to one factor and are often connected to multiple factors such as implicit bias. However, by having bias awareness, biased thinking can be recognized before it can negatively impact medical decision-making.
Resources
¹Clinician-identified problems and solutions for delayed diagnosis in primary care: a PRIORITIZE study - PMC (nih.gov)
²https://www.plaxenadler.com/2023/02/21/the-largest-medical-malpractice-…
³https://www.law.com/thelegalintelligencer/2022/10/06/jury-hands-up-19-7…
4https://mediaconnect.com/jury-verdict-for-33-year-old-tom-bosworth-is-l…
5Reducing delay in diagnosis: multistage recommendation tracking. | PSNet (ahrq.gov)
6The systems approach at the sharp end - PMC (nih.gov)
7Tackling Implicit Bias in Health Care | NEJM
8What Is Implicit Bias, How Does It Affect Healthcare? (patientengagementhit.com)
9Quick Safety 23: Implicit bias in health care | The Joint Commission